Opioids: How Settlement Dollars Advance City and County Opioid Abatement

Author
Upcoming Events
Related News
Building on a strong history of collaboration, including the National City-County Task Force on Opioids, NACo and the National League of Cities examined preliminary data on the distribution of opioid settlement dollars across cities, counties and states. This brief highlights how cities and counties are working together to abate the overdose crisis, including pooling opioid settlement funds to create a more comprehensive system of care for people with substance use disorder.
Download the brief to learn about the allocation of opioid settlement funds between cities, counties and states and how cities and counties are coordinating to maximize the impact of these funds.
About the Brief
Building on a strong history of collaboration, including the National City-County Task Force on Opioids, NACo and the National League of Cities examined preliminary data on the distribution of opioid settlement dollars across cities, counties and states. This brief highlights how cities and counties are working together to abate the overdose crisis, including pooling opioid settlement funds to create a more comprehensive system of care for people with substance use disorder.
Download the brief to learn about the allocation of opioid settlement funds between cities, counties and states and how cities and counties are coordinating to maximize the impact of these funds.
The Opioid Crisis in the United States
The opioid crisis continues to be a significant public health concern, with opioid-involved overdose deaths nearly quadrupling between 2010 and 2021, including from synthetic opioids like fentanyl.1 However, there has been progress in addressing the issue, with multiple financial settlements awarded to states, counties and municipalities as redress for the harms caused by pharmaceutical companies in creating this epidemic.
Building on the strong history of collaboration, including the National City-County Task Force on Opioids, the National League of Cities (NLC)
and the National Association of Counties (NACo) together are working to empower cities and counties to invest these funds in life-saving strategies and to highlight opportunities to collaborate on addressing their shared concerns around this epidemic.
In this brief, we examine the total dollars awarded from the first, and largest, of the national opioid settlements; their distribution across cities, counties and states; and highlight several ways in which cities and counties are working together to address the ongoing crisis using these funds, including pooling resources together to support more comprehensive approaches to improve individual and community outcomes.
History and Settlements
For the first fifteen years of the 21st century, prescription opioids were involved in more overdose deaths than any other substance in the
U.S. Nearly 180,000 people died of a prescription opioid-involved overdose in this period, which is more than the population of Charleston, S.C. In addition to its devastating societal effect, the opioid epidemic created an enormous need for a range of public services, from emergency medical services to legal investigations.
Between 2016 and 2020, local governments filed thousands of lawsuits against pharmaceutical companies to resolve their liabilities in creating the opioid epidemic. In 2021, a coalition of state attorneys general, led by an executive committee of 14 states, negotiated a nationwide settlement with opioid manufacturer Johnson & Johnson and distributors AmerisourceBergen, Cardinal Health and McKesson.2 Intergovernmental cooperation was critical to this process: to unlock the full payout, 90 percent of cities and counties in each state needed to surrender their individual cases and join their state agreements. Cities, counties and states came together to reach this milestone and by early 2022, a settlement of $26 billion was finalized.
The opioid multidistrict legislation (MDL) began more than 5 years ago, before Judge Dan Polster, and now encompasses more than 3,000 local governments. Judge Polster established various bellwether cases to assess the merits of claims against the three major classes of defendants— manufacturers (Purdue, Mallinckrodt, J&J, and others), distributors (McKesson, Cardinal, AmerisourceBergen, and others), and pharmacies (CVS, Rite-Aid, Walgreens, Walmart, and others). While this brief covers the largest of the opioid settlements, these cases and their results are important to the many other jurisdictions who have not yet settled, including those who continue to fight for remand in state court.
The $26 billion settlement represents the first, and largest, of the national opioid settlements. As of June 2023, cities, counties and states have achieved over $50 billion in opioid settlement payments. How these funds are allocated between state and local governments varies across states and settlement agreements. In this brief, NLC and NACo examine how funds from the $26 billion settlement were allocated across each level of participating government (i.e., state, city and county) and highlight examples of continued intergovernmental collaboration.
Distribution of Settlement Dollars
How Much Money are States, Counties and Cities Getting?
As of July 2023, intrastate allocation formulas were available for 45 out of 50 states. The available data comprises $20 billion of the $26 billion national settlement. As shown in Figure 1, 50 percent of all funding is going directly to states (approximately $9.7 billion).
The remainder is allocated between counties and cities; counties will receive approximately $7.3 billion (38% of total funds) while cities will receive approximately $2.4 billion (12% of total funds).
Importantly, no set of allocations was the same across these localities, such that some cities received $0 (see Methodology section for details) while others received as much as $2.5 million over 18 years. The average amount awarded to the 7,529 cities was approximately $690 thousand.
Of the 2,769 counties receiving funds, they received an average of $3.15 million with some receiving as much as $24 million over 18 years. Notably, in some states, counties receive the majority of the funds (e.g., North Carolina).
How Many Cities and Counties are Receiving Settlement Funds?
Cities and counties received direct distributions in all states, except for Alabama, Delaware and Louisiana where the distributions were combined across the state and local levels.3 In states where funds were clearly awarded to local governments, the majority of funds were directly distributed to counties (covering 2,769 counties out of a nationwide total of 3,069 counties).
Funds also went to 7,529 cities though cities received lower amounts on average than counties. This distribution is largely due to counties covering larger geographic portions of each state and often serving as the governmental home for public health agencies.
Figure 2 | Percent of Municipalities Receiving Opioid Settlement Funds by State
On average, 32 percent of cities receive settlement funds in each state
Source: Data are drawn from settlement documentation MOUs and the U.S. Census of Governments.
Note: Data represents 45 states; AL, CO, DE, LA and NV are not included due to missing data at the county/city level.
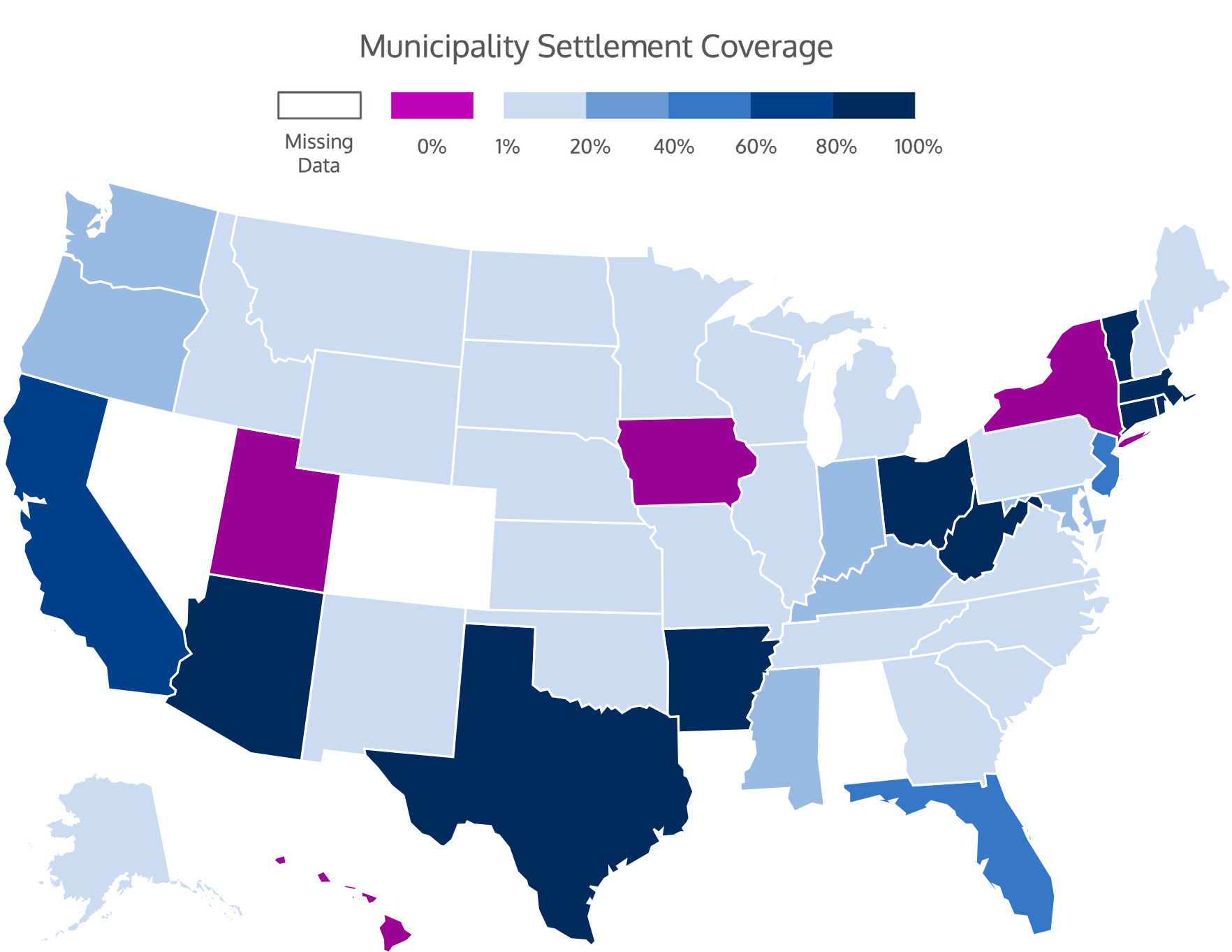
Figure 3 | Percent of Counties Receiving Opioid Settlement Funds by State
In most states, all counties receive settlement funds
Source: Data are drawn from settlement documentation MOUs.
Note: Each state has a different number of counties; these data reflect unadjusted numbers of counties. Data represents 45 states; AL, CO, DE, LA and NV are not included due to missing data at the county/city level.

Partnerships
How are Counties and Cities Partnering to Use Their Funds?
Clinton County and City of Frankfurt, Ind.
Indiana’s Clinton County and the City of Frankfort came together to make the most of their opioid settlement funds. They first created a joint Opioid Settlement Funding Committee, comprised of city and county officials, first responders, health department representatives and mental health organization stakeholders from across the county.4 The settlement committee conducted a community needs assessment to identify gaps in services. Funds will be allocated to evidence-based prevention, treatment, recovery, harm reduction, behavioral health workforce, enforcement, jail treatment, recovery residences and other services. Clinton County and the City of Frankfort have worked “hand-in-hand” to create cross-cutting programs and break down silos.
New Hanover County and City of Wilmington, N.C.
The joint opioid committee, formed by New Hanover County and the City of Wilmington in December 2022, aims to tackle the opioid crisis through a collaborative approach. The committee’s proposed plan focuses on three main categories, including education and outreach, access to services and treatment for sustainable recovery and well-being.5 Recommendations are then approved in separate meetings by the city council and board of commissioners. By forming a joint opioid committee that includes both elected officials and staff, New Hanover County and the City of Wilmington are pooling their resources and expertise to develop a comprehensive and holistic approach.
Arkansas Opioid Recovery Partnership (ARORP)
The Arkansas Opioid Recovery Partnership (ARORP) was founded in 2022 by the Arkansas Municipal League and the Arkansas Association of Counties. The goal of this collaborative approach is to combat the opioid epidemic in Arkansas by creating a united front of local government representatives. This innovative approach allows local governments to pool their resources to create a more effective response to opioid use disorder. ARORP offers funds for applicants applying for general funds, as
well as overdose response teams and naloxone distribution. The ARORP website has detailed information on how to apply for these funds, including eligibility criteria and the application process.6 The website also has a section dedicated to tracking the progress of funded projects, which provides transparency and accountability to the community.
Conclusion
Where Do Cities and Counties Share Opportunities and Challenges?
Though critically needed, for most cities and counties, incoming settlement payments pale in comparison to opioid-related costs. An analysis of public expenditures from 20 cities and counties across the country found that for every three overdose deaths, public safety expenditures increase by $130,000-$140,000.7 Identifying promising and right-sized investments requires precise planning, which
is challenging when the amount and timeline of payments varies each year. In many states, the initial rollout of settlement funds involved unexpected delays and even surprises in the amount of deposits, which presents the risk that future payments will be adjusted to account for these differences. Another challenge is the amount of opioid settlement payments relative to the growing costs of the opioid epidemic.
The number of opioid-involved overdose deaths has more than doubled since 2015: In 2021, annual overdose deaths topped 100,000 for the first time in American history.8 With half of opioid settlement funds allocated to states, local governments must deploy these finite funds against an evolving crisis.
To ensure opioid settlement funds make the greatest possible difference in local communities, cities and counties are working creatively and collectively to administer these funds. Some cities and counties are pooling funds to finance more costly expenses, such as construction costs for substance use service facilities. Cities and counties are also creating coordinating committees or joint planning bodies to ensure expenditures within each locality help close service gaps that persist across geographic boundaries. In these ways and more, cities and counties are leveraging their individual assets and expertise to support one another in abating the opioid epidemic.
Community members are one of the most important assets our local governments can leverage in this process. By engaging with residents and understanding their unique perspectives and experiences, local governments can better target their efforts and develop programs that are effective, culturally relevant and financially feasible. There are multiple low cost, high impact abatement strategies that could be implemented or expanded using opioid settlement funds, and local governments can engage local stakeholders to ensure funding decisions address the needs of people with substance use disorders.
Featured Initiative
Opioid Solutions Center
NACo's Opioid Solutions Center empowers local leaders to invest resources in effective treatment, recovery, prevention and harm reduction practices that save lives and address the underlying causes of substance use disorder.

Endnotes
- National Institute of Health (2023, February 9). Drug Overdose and Abuse National Institute on Drug Abuse. Retrieved May 25,2023, from https://nida.nih.gov/research-topics/ trends-statistics/overdose-death-rates
- OpenGov (n.d.). Quantifying How Much the Opioid Epidemic Costs Governments. The OpenGov Research Team. Retrieved May 25, 2023, from https://stories.opengov. com/jwu-demo/published/SJ0phpWkm
- These states are excluded from subsequent analyses due to missing or unsubstantiated data. Alabama received dollars to the state and local levels but the local levels are not distinguished due to missing data and thus Alabama is also removed from subsequent analyses. See Methodology section for more detail.
- Healthy Communities of Clinton County (n.d.). City and County Officials working together to better Frankfort’s Recovery Community. Frankfort, Indiana Government. Retrieved May 25, 2023, from https://frankfort-in.gov/ egov/documents/1675457722_33052.pdf
- Mojica, (2022, December 12). Joint Opioid Committee lays out spending plans for Wilmington and New Hanover County at latest meeting. WHQR.org. Retrieved May 25, 2023, from https://frankfort-in.gov/egov/ documents/1675457722_33052.pdf
- Arkansas Opioid Recovery Partnership (n.d.). About ARORP.org. Retrieved May 25, 2023, from https://frankfort-in.gov/egov/ documents/1675457722_33052.pdf
- National Association of Attorneys General (n.d.). NAAG.org. Retrieved May 25, 2023, from https://www.naag.org/issues/opioids/
- Centers for Disease Control and Prevention (2023, February 15). Provisional Drug Overdose Death Counts. National Center for Health Statistics. Retrieved May 25, 2023, from https://www.cdc. gov/nchs/nvss/vsrr/drug-overdose-data.htm
- The Lebanon Reporter (2023, March 7). Clinton County, Frankfort lauded for opioid settlement plan. Retrieved May 25, 2023, from https://www.reporter.net/news/ local_news/clinton-county-frankfort-lauded- for-opioid-settlement-plan/article_6f049df2- b9e4-11ed-b3a9-f3c82cb63315.html
Acknowledgements
This work is a collaboration between the National League of Cities (NLC) and the National Association of Counties (NACo). To learn more about resources available to counties to maximize the impact of opioid settlement funds, visit NACo’s Opioid Solutions Center. Additionally, we thank the multiple colleagues at NLC and NACo who reviewed and provided feedback on this brief.
Methodology
This analysis was driven by data collected from publicly available settlement data gathered between February and April 2023. Dollars allocated by government type were collected individually by state, then separated and aggregated for totals. Notably, three states (Alabama, Delaware and Louisiana) did not have specification for distribution to local governments and thus are excluded from this analysis. Colorado had a variety of distributions to local governments and regions; however, lack of clarity
in the memorandum of understanding prevented their inclusion in the analysis. Also of note, in Iowa, New York and Utah no cities were awarded funds. Connecticut and Rhode Island have no county governments and therefore counties were not awarded any funds. The settlement dollars have been awarded by the following companies:
Opioid manufacturer, Johnson & Johnson ($5 billion)
The “Big Three” opioid distributors McKesson, AmerisourceBergen, and Cardinal Health ($21 billion)







