Funding Strategies for County Behavioral Health Crisis Care

Upcoming Events
Related News
America’s 3,069 counties are a cornerstone of the nation’s health systems, investing over $80 billion annually in community health, which includes crisis care services. County-based behavioral health programs operate in 23 states, serving 75 percent of the U.S. population. Counties also deliver Medicaid-eligible services and assist with bridging funding gaps in administering the program. By providing wrap-around human services supports such as housing assistance, employment services, and food security programs, counties strengthen crisis care and ensure timely community-based support for individuals facing mental health and substance use challenges.
County-based behavioral health programs operate in 23 states
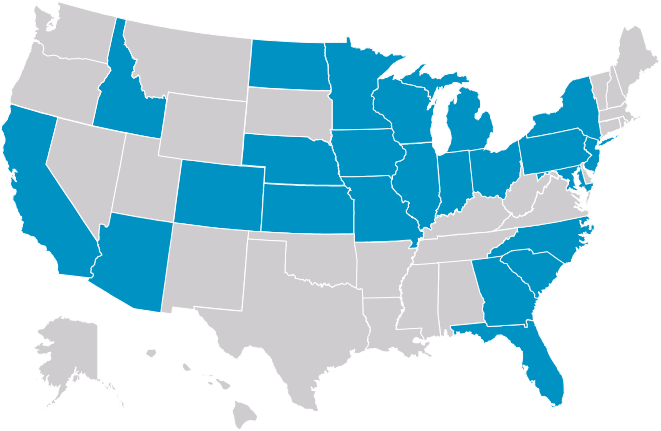
America’s 3,069 counties are a cornerstone of the nation’s health systems, investing over $80 billion annually in community health, which includes crisis care services. County-based behavioral health programs operate in 23 states, serving 75 percent of the U.S. population. Counties also deliver Medicaid-eligible services and assist with bridging funding gaps in administering the program. By providing wrap-around human services supports such as housing assistance, employment services, and food security programs, counties strengthen crisis care and ensure timely community-based support for individuals facing mental health and substance use challenges.
Counties can leverage diverse funding streams and intergovernmental and cross-sector partners to improve coordination of care for individuals with mental illness and substance use disorders.
Primary Behavioral Health Funding Streams
Creative Funding Strategies
Counties across the country are developing innovative strategies to fund behavioral health care.
Blending occurs when financial resources from various funding streams are combined into a unified pool of commingled funds to support an initiative or acquire specific services.
Braiding combines multiple funding streams to provide specific services simultaneously, requiring interagency coordination and collaboration.
Sequencing organizes different sources of funding to separate and sequentially provide specific services.
Reducing Barriers
Counties are applying a variety of creative solutions to overcome barriers to behavioral health care funding.
Strategy
Counties can blend, braid and sequence various funding sources from federal, state and local governments, as well as private grants and donations.
County in Action
Missoula County, Mont. leverages funding from Montana's HB 872, which includes a historic $300 million investment in behavioral health and developmental disabilities service systems. This bill supports the Behavioral Health Systems for Future Generations initiative aimed at enhancing infrastructure, improving access to care, and ensuring long-term sustainability.
Strategy
Leverage state and federal funding sources, such as Medicaid, IMD waivers and opioid settlement funds to cover the cost of care while working to establish comprehensive insurance reimbursements through state, federal and private collaboration.
County in Action
Middlesex County, Mass., leverages the MassHealth Behavioral Health Initiative to fund Community Behavioral Health Centers (CBHCs) through a Medicaid 1115 demonstration waiver, which enhanced reimbursements for outpatient and crisis care. With this state tool, the county is further supporting expanded mobile crisis and preventive services, thereby reducing dependence on costly emergency and inpatient care.
Strategy
Encourage community involvement to increase awareness and support for behavioral health initiatives, which can result in additional funding through local fundraising efforts, non-profit or community organization resources and philanthropic donations.
County in Action
In 2022, The Leona M. and Harry B. Helmsley Charitable Trust awarded a $4 million grant to Pivot Point, the Pennington County (S.D.) Crisis Stabilization Unit to fund the first 36 months of operations in the new facility.





