From Crisis to Solutions: Policy Catalysts for Improved Outcomes

Upcoming Events
Related News
As leaders of America’s counties, we call for urgent action – a new vision – on how we, as a prosperous and creative nation, promote the mental health and wellbeing of our communities and people, especially those who need more access to quality care and treatment.
Jump to Section
- National Landscape: A Case for Action
- Letter from Commission Co-Chairs
- List of Commission Members
- Timeline: Commission Achievements & Milestones
- Summary of Proposed Federal Policy Reforms
- A New Vision for Mental Health and Wellbeing
- Policy Priorities
- Additional Focus Areas
- Next Steps for County Officials
- Download Full Report
A Call From the Frontlines for National Action
Our nation’s mental health policies and practices require meaningful leadership and reforms to address the severity and immediacy of today’s mental health crisis.
The National Association of Counties (NACo) Commission on Mental Health and Wellbeing reflects the vision and commitment of America’s county leaders to be a catalyst for immediate national action. With 75 percent of the U.S. population relying on county-based behavioral health services, county leaders are on the frontlines of today’s challenges: mounting caseloads, declining resident outcomes, falling workforce productivity and increasing costs across all sectors.
County officials across the country are demanding reforms to improve the wellbeing of residents, use resources more wisely and coordinate care for people suffering from mental illness. We are investing our capital – financial, political and social – into making these essential changes. We call on our intergovernmental and cross-sector partners to join us.
Over the past year, the Commission on Mental Health and Wellbeing has worked to:
- Stimulate a national sense of urgency, through an intergovernmental partnership framework, to address our nation’s mental and behavioral health crisis,
- Elevate national awareness of the roles, innovations and pain points facing county governments and our partners in addressing this escalating crisis,
- Advance public policy goals to increase access to care, coordinate a continuum of care and build the mental health workforce of the future, and
- Align a cohesive national intergovernmental and cross-sectoral strategy to improve and enhance the mental health and wellbeing of all Americans, with a special focus on our most vulnerable populations.
Our Why: Defining the National Crisis
- Almost one in four U.S. adults aged 18 or older experience any mental illness (AMI) each year, 26 percent experiencing a serious mental illness that substantially interfered with or limited major life activities. One in 12 had co-occurring AMI and substance use disorder (SUD).1
- Nearly one in five adolescents aged 12 to 17 experienced a major depressive episode (MDE) in 2022, with 20 percent having co-occurring MDE and SUD.2
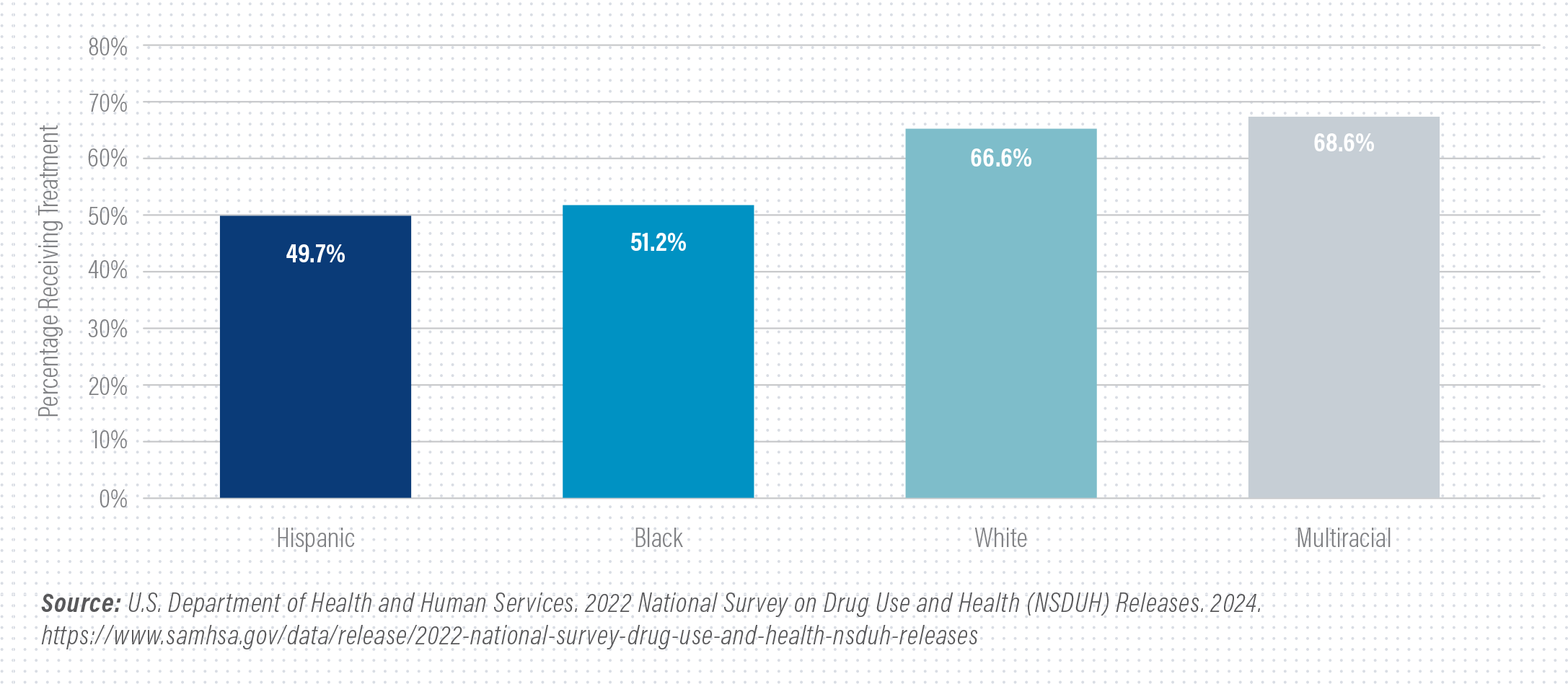
- In 2022, white and multiracial adults were more likely to receive mental health services in the past year than Black, Hispanic or Latino, or Asian adults.3
- Nearly a quarter of American adults in 2022 took prescription pills for mental health, up from only 15.8 percent in 2019.4
- Suicide is now the second leading cause of death among individuals between the ages of 10-14 and 25-34, and the third leading cause of death among individuals between the ages of 15-24.5
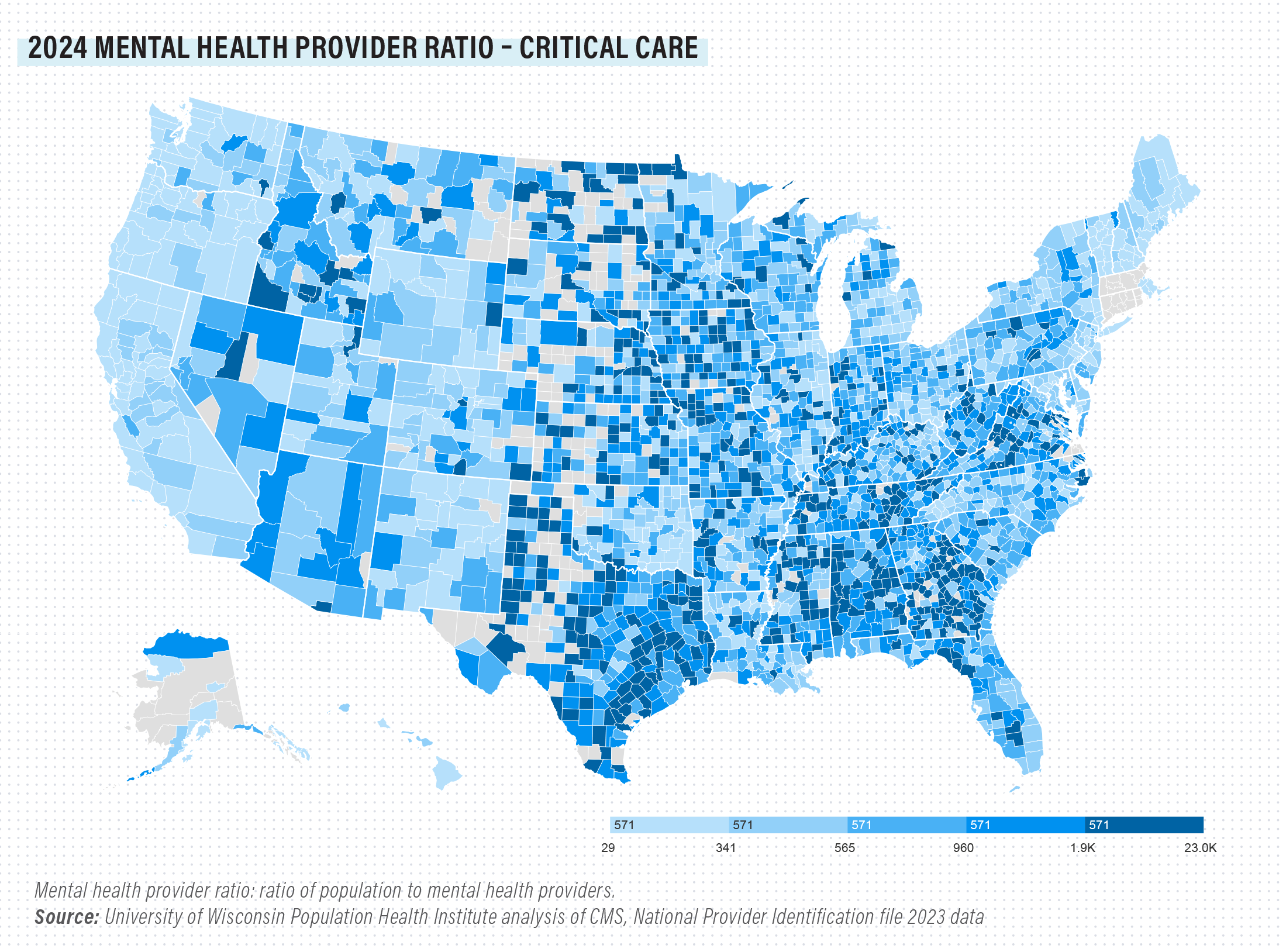
- One-third of the U.S. population lives in a county designated as a mental health professional shortage area.6
- Serious mental illness causes $193.2 billion in lost earnings each year across the U.S. economy, with substance use disorders resulting in more than $740 billion annually in additional lost workplace productivity, health care expenses and crime-related costs.7
Letter from Commission Co-Chairs

Hon. Kathryn Barger

Hon. Dow Constantine
Letter from Commission Co-Chairs
The impact of the current mental health crisis is felt deeply across America’s 3,069 counties. By making substantial investments in community health systems, hospitals, human services and public safety systems, counties play an indispensable role in the efforts to alleviate this struggle.
In February 2023, the National Association of Counties (NACo) established the Commission on Mental Health and Wellbeing, rallying county officials and our partners to confront our nation’s escalating crisis. As county leaders, we have advocated tirelessly for accountability, flexibility, incentives and reforms that promote better outcomes, optimize resources, foster collaboration and encourage compassion.
Over the last year, the Commission made considerable progress through strategic policy advocacy and collaboration with federal, state and community leaders. Our efforts focused on four foundational policy priorities:
- Fortifying local crisis response systems
- Rectifying exclusionary Medicaid policies
- Bolstering the mental health workforce
- Ensuring mental health parity enforcement
These policy priorities serve as beacons in our collective mission to foster healing and resilience across all communities and regions. As custodians of our communities’ physical and mental wellbeing, it is our duty to prioritize appropriate, equitable and effective resources for those most in need. Together, we can bridge gaps, empower individuals and create lasting wellness for all.
The following report delves into the four policy priorities identified by our commission, presenting federal policy recommendations designed to address the acute mental health crisis in America and offering practical solutions for county leaders and our partners.
We know that we are just getting started on this journey and look forward to partnering with you to help our residents and our communities thrive.
Hon. Kathryn Barger
Los Angeles County, Calif.
Commission Co-Chair
Hon. Dow Constantine
King County, Wash.
Commission Co-Chair
About the Commission
Commission kicked off work in partnership with the Department of Health and Human Services (HHS) and the Substance Abuse and Mental Health Services Administration (SAMHSA) Leadership
Launched Mental Health Awareness Month with new county-level data on the scope of the U.S. mental health crisis and an outline of four policy focus areas
Outlined priorities for workforce development with the National Association of County Behavioral Health and Disability Directors (NACBHDD)
Partnered with the White House, HHS and the Department of Labor (DOL) officials on the development of regulatory reforms to mental health parity enforcement
Secured key priorities in the Congressional Bipartisan Mental Health and Substance Use Disorder Taskforce Policy Agenda
Secured reforms to federal Institutions for Mental Diseases (IMD) exclusion and state Medicaid termination policies in fiscal year (FY) 24 Appropriations Minibus Package
Secured FCC regulatory reforms that will make the 988 Suicide & Crisis Lifeline more accessible to callers in crisis and need
Provided consultation to SAMHSA, the Health, Resources and Services Administration (HRSA), the Department of Justice (DOJ), the Administration for Community Living (ACL) and the Centers for Medicare & Medicaid (CMS) on updating federal guidance on crisis
Formed partnership with the National Alliance on Mental Illness (NAMI) to call on Congress to pass critical substance use disorder legislation
CO-CHAIRS
Hon. Kathryn Barger
Supervisor, Los Angeles County, Calif.
Hon. Dow Constantine
County Executive, King County, Wash.
MEMBERS
Dr. April Aycock
Director, Office of Mental Health, Monroe County, N.Y.
Hon. Mary Ann Borgeson
Commissioner, Douglas County, Neb.
Hon. Therese Brown
Commissioner, Allen County, Ind.
Dr. Kathleen Burke
Will County Health Department, Will County, Ill.
Hon. David Crowley
County Executive, Milwaukee County, Wis.
Hon. Bryan Davis
Commissioner, Scioto County, Ohio
Hon. Jerry Demings
Mayor, Orange County, Fla.
Hon. Adrian Garcia
Commissioner, Harris County, Texas
Hon. Clay Jenkins
Judge, Dallas County, Texas
Hon. Steven Leifman
Judge, Miami-Dade County, Fla.
Dr. Gina Nikkel
Executive Director, Association of Oregon Counties
Hon. Helen Stone
Commissioner, Chatham County, Ga.
A crisis that affects the whole country requires solutions that involve different levels of government and sectors. We respectfully urge federal policymakers to keep working with us to enhance mental health policies and resources for people throughout all our communities. We can achieve better outcomes with our regional and local efforts when we work together among and across the public, private and nonprofit sectors.
The following recommendations, organized around four policy pillars, call for federal actions that complement and enhance our efforts at the county level.
- Remove federal limitations under Medicaid, Medicare, the Children’s Health Insurance Plan (CHIP) and the Department of Veterans Affairs on benefits for persons in jail custody pending disposition of charges.
- Expand the approval of federal regulatory measures and advance federal policy to allow Medicaid payment for medical services furnished to any eligible incarcerated individual during the period that proceeds the individual’s release.
- Waive IMD regulatory restrictions for adults with serious mental illness (SMI), children with serious emotional disturbance and short-term residential stays for the treatment of substance use disorder (SUD).
- Waive IMD restrictions, either by legislative or regulatory action, for short-term crisis stabilization facilities.
- Coordinate resources and technical assistance to local governments on the development of crisis call centers.
- Fund programs that aid in the development, expansion and sustainment of crisis response infrastructure, a major shortfall in today’s system of care.
- Expand evidence-based crisis response models, including crisis intervention team (CIT) programs and Assistance Helping Out on The Streets (CAHOOTS).
- Authorize Medicaid financing for regional and local crisis call center operations, crisis stabilization facilities and integrated primary, mental health and crisis response care models such as Certified Community Behavioral Health Clinics (CCBHC).
- Create clear entry pathways for behavioral health professions, particularly in rural and underserved areas, using a comprehensive approach (e.g., stipends, loan forgiveness program, streamlining licensure/credentialing processes, tax incentives, etc.).
- Increase funding for existing programs, such as the National Health Service Corps, that promote workforce recruitment and retention in local underserved areas.
A New Vision for Mental Health and Wellbeing
Our mission is clear: modernize today’s mental health policies and practices to meet the scale and urgency of the moment.
As a world leader in healthcare innovation, counties can compassionately enhance resident results, address mounting caseloads, improve workforce productivity and reduce costs across all sectors.
The Commission on Mental Health and Wellbeing embodies a steadfast commitment to tackling mental health challenges holistically, as we increase equitable access to services, reduce stigma and build more resilient communities.
As leaders of America’s counties, we call for urgent action – a new vision – on how we, as a prosperous and creative nation, promote the mental health and wellbeing of our communities and people, especially those who need more access to quality care and treatment.
A Call for Action
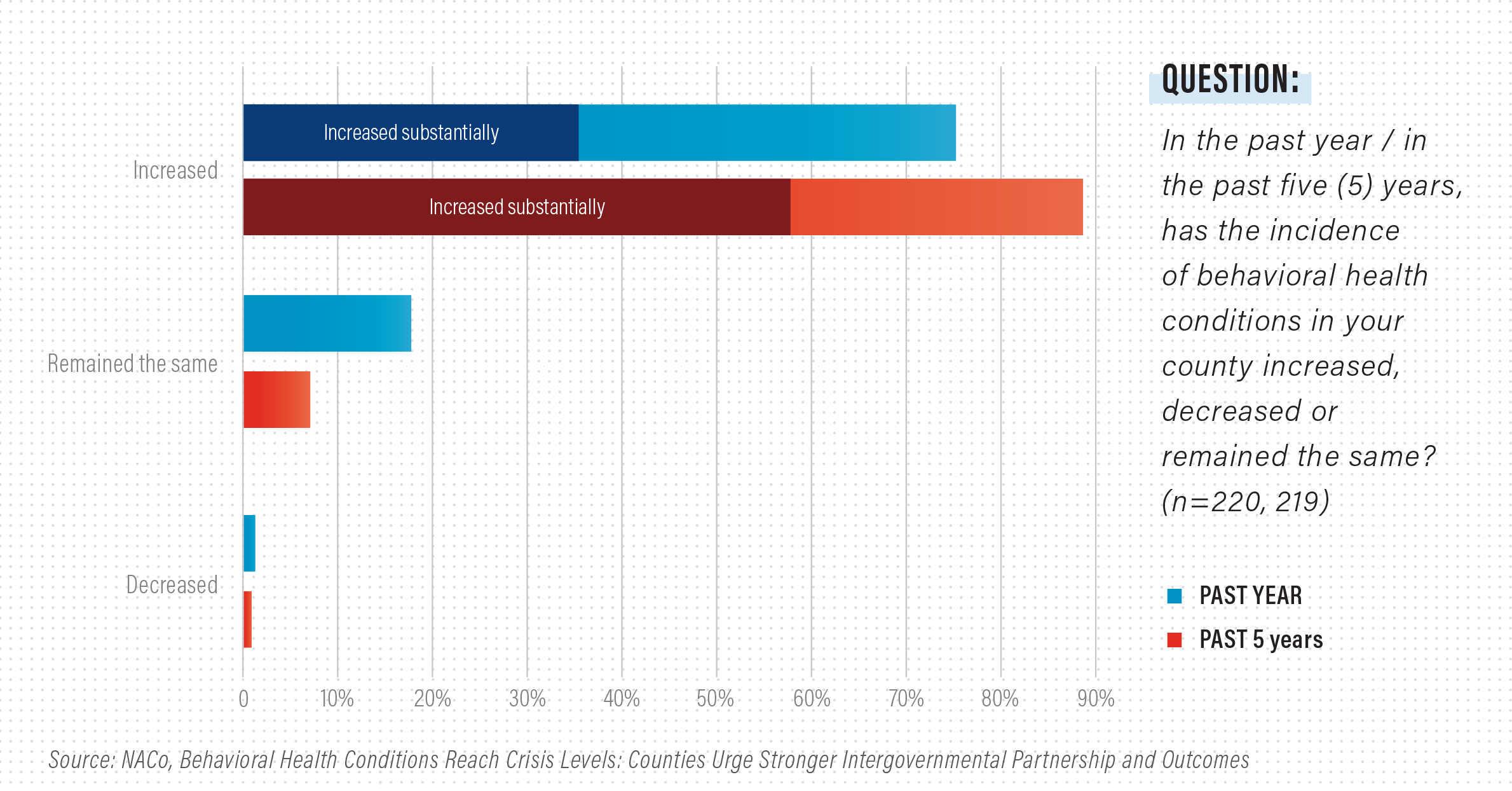
Our nation faces an escalating crisis in behavioral health, a challenge that reverberates through every corner of society. NACo members report a staggering 75 percent surge in behavioral health conditions in the past year, with nearly 90 percent of counties reporting a marked increase over the past five years. This crisis isn’t confined to adults alone, manifesting in youth as issues of violence, substance abuse, mental illness and safety concerns.
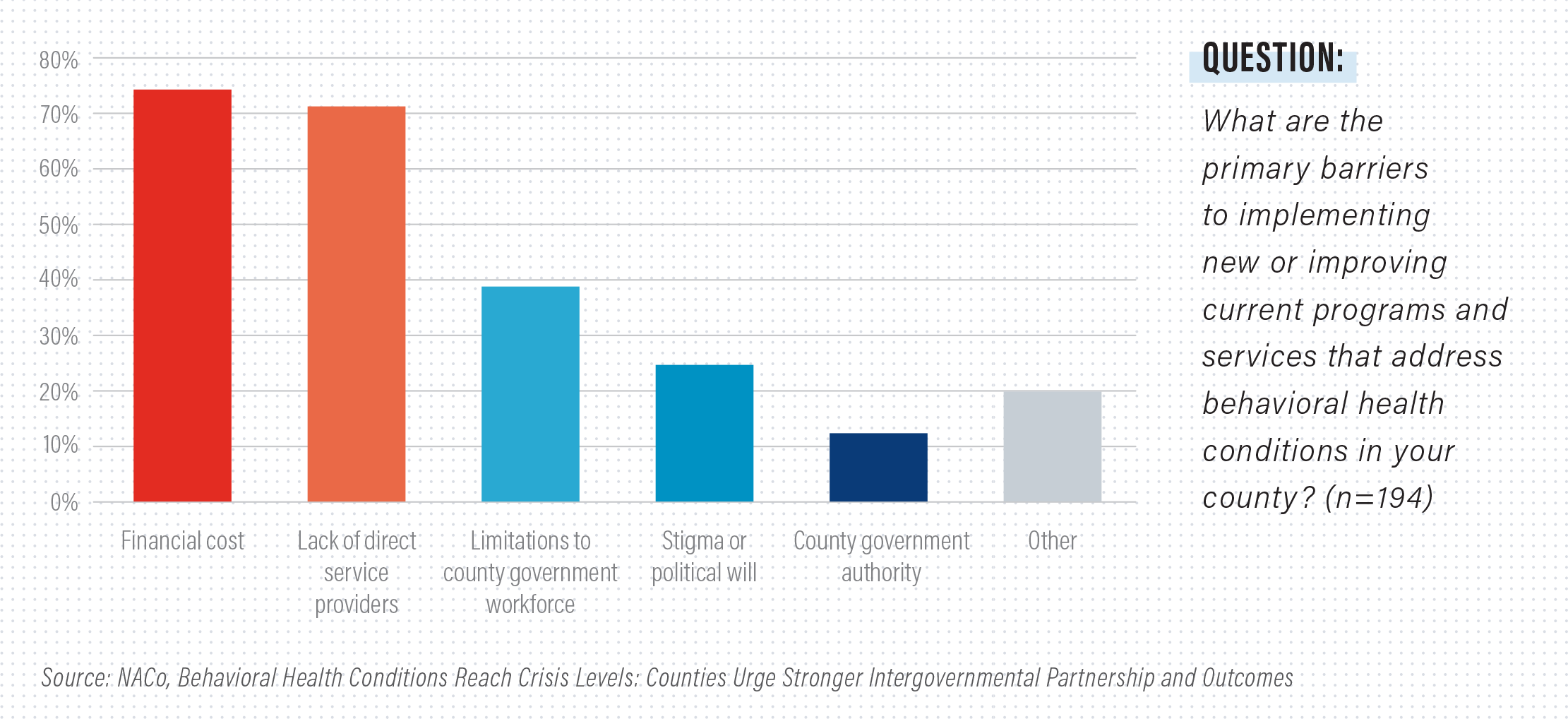
County leaders are acutely aware of the mental health crisis and are actively working to implement policies and practices aimed at enhancing prevention and crisis response through collaborative systems of care. Yet a major shortage of direct service providers, coupled with federal policy barriers and misaligned incentives for better care, poses formidable challenges.
The mental health crisis is not merely a collection of isolated incidents but a pervasive challenge that permeates entire communities. Counties are looking for ways to improve access, reduce wait times and strengthen mental health care delivery and response systems. To make sustainable improvements in the state of our nation’s mental health, we need strong partnerships and collaborat
Policy Overview: The Medicaid Inmate Exclusion Policy (MIEP)
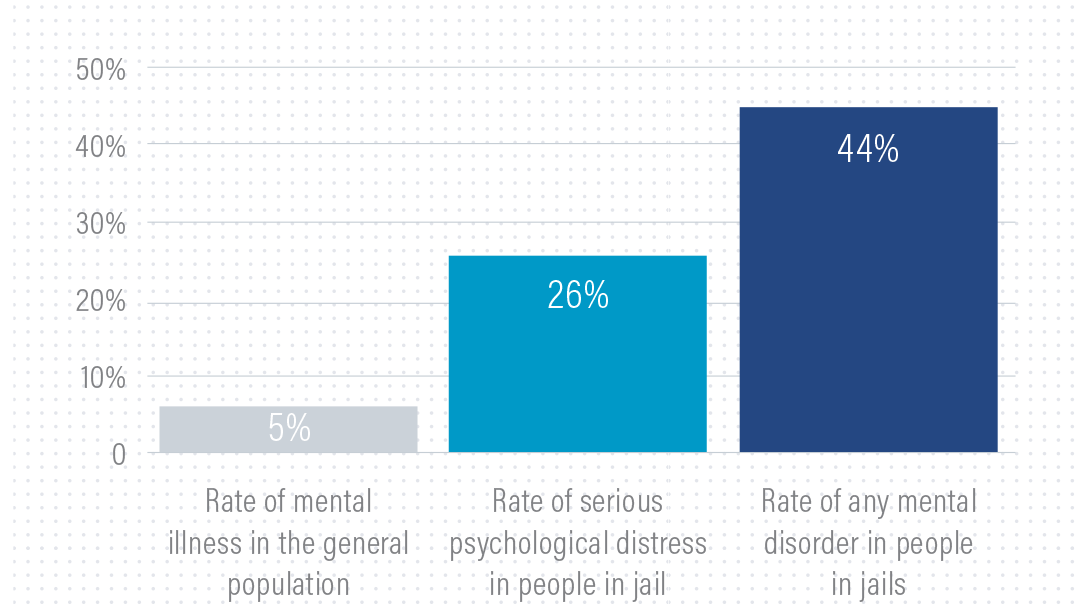
People in Jails Have Disproportionate Rates of Mental Illness
The Medicaid Inmate Exclusion Policy (MIEP) is a federal policy outlined under Section 1905(a)(A) of the Social Security Act that revokes federal health benefits for adults and juveniles housed in correction institutions – making no distinction between individuals who are being detained in jails prior to due process, versus individuals who have been adjudicated and sentenced to time in a jail or prison.
Without revision, this policy creates inequitable and unconstitutional disruptions to primary and behavioral health care services for justice-involved people, exacerbating rates of untreated mental illness and substance use disorder in local communities and increasing rates of jail recidivism.
The most recent national data indicate that one in four people detained in jails (26 percent) reported experiences that met the threshold for serious psychological distress and 44 percent had been told in the past by a mental health professional that they had a mental disorder.8
Amending the MIEP to allow individuals who are detained pretrial to retain access to Medicaid and other federal health benefits would help break the cycle of recidivism exacerbated by untreated physical and mental illnesses and substance use disorders.
Without revision, MIEP creates inequitable and unconstitutional disruptions to primary and behavioral health care services for justice-involved people, exacerbating rates of untreated mental illness and substance use disorder in local communities and increasing rates of jail recidivism.
Section 1905(a)(30)(B) of the Social Security Act prohibits Medicaid funds from covering an individual’s care at an institution of mental disease (IMD), defined as a facility with more than 16 beds with the primary function to diagnose or treat people with behavioral health disorders. This policy, referred to as the IMD exclusion, limits a county’s ability to build health care systems that adequately serve our communities. It also perpetuates patient inequities by limiting access to services in the most appropriate settings.
The IMD exclusion was created as part of the deinstitutionalization movement, which shifted responsibility for funding inpatient psychiatric services from the federal level to individual states.9 While localized control was intended to protect patients from maltreatment that too frequently occurred due to mass institutionalization, the policy instead greatly reduced access to quality care.
By severely restricting Medicaid reimbursement for inpatient facilities that serve populations greater than 16, large population centers are disempowered from administering adequate behavioral health care. Though the demand for behavioral health care is growing, capacity is not. Modernizing the Medicaid IMD exclusion with safeguards and quality standards would significantly increase the treatment capacity of county-operated hospitals and behavioral health facilities while also promoting equitable access to treatment options for our most vulnerable residents.
Learn more about how the IMD exclusion impacts counties
Since February 2023, NACo’s Commission on Mental Health and Wellbeing continues to make important incremental progress in reforming Medicaid policies that create barriers to behavioral health treatment. Highlights include:
- Secured access to Medicaid and Children’s Health Insurance Program (CHIP) benefits for justice-involved youth in pretrial status: The fiscal year (FY) 2023 Omnibus Appropriations Package included crucial provisions allowing these young individuals to maintain Medicaid and CHIP benefits while in pretrial status and for 30 days prior to release, ensuring continuity of care during these critical periods.
- Secured reforms to the federal IMD exclusion and state Medicaid termination policies: The FY 2024 Minibus Appropriations Package permanently waived the IMD exclusion for substance use disorder treatments, allowing state Medicaid programs to receive federal reimbursement for up to 30 days of inpatient substance use disorder treatment provided for an individual in an IMD facility. It also mandated that states suspend, rather than terminate, Medicaid benefits upon arrest, ensuring continuous healthcare coverage for affected individuals.
- Achieved policy alignment with congressional stakeholders: As a result of the Commission’s direct engagement with key congressional stakeholders, two crucial bills were included in the Congressional Bipartisan Mental Health and Substance Use Disorder Task Force’s 2023 agenda. These bills are essential for securing Medicaid access for individuals in pretrial detention and those reentering communities. Additionally, in a November 2023 letter to Senate committees, the Commission outlined key policy priorities for upcoming mental health legislation, urging Congress to reauthorize the SUPPORT Act and advance vital behavioral health policies, demonstrating our ongoing commitment to these critical issues.
Los Angeles County is finding creative ways to support its large population with diverse behavioral health treatment needs and still be in compliance with federal restrictions. But due to those federal restrictions, these reforms come at a great cost to the county, taxpayers and patients.
Subacute behavioral health facilities offer inpatient services that are less intense than those required for severe illnesses needing acute hospitalization but more intense than conditions requiring partial or no hospitalization. These facilities focus on short-term, intensive, recovery-oriented services to stabilize patients, especially those whose conditions are too severe for outpatient care. The facilities also provide a stable environment for individuals without housing during the treatment period.
In 2019, the Los Angeles County Department of Mental Health reported a shortage of 3,000 subacute mental health beds. As a result, patients remained in acute inpatient facilities for two months or longer awaiting appropriate placement. In total, approximately three-quarters of all county Department of Health patients are awaiting placement in lower-level care facilities and receiving minimal to no reimbursement for the associated cost. Despite growing needs for subacute beds, increasing the supply is difficult under the IMD exclusion policy’s 16-bed limit.
Despite the evident disparity in treatment provisions and the increased financial burden, Los Angeles County leaders remain steadfast in their commitment to addressing the mental health crisis. By navigating the complexities of IMD exclusions, county leaders continue to seek innovative solutions to provide essential behavioral health services to those in need.
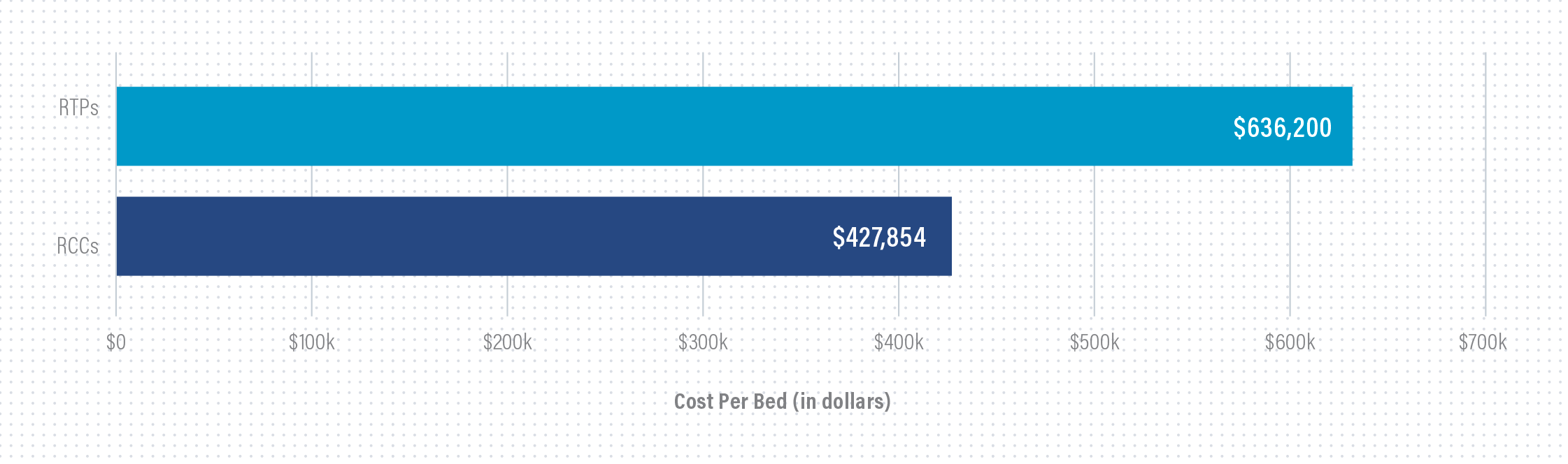
To meet local demand and remain compliant with federal IMD restrictions, the county spread 80 subacute beds across five residential treatment program facilities (RTPs). Conversely, Los Angeles County’s physical health Recuperative Care Center (RCC) is a single facility with 48 beds.11 The approximate cost per bed in the RTPs was $636,200, nearly 1.5 times the RCC cost per bed ($427,854). Separate buildings for intensive behavioral health treatment significantly increase construction costs and create operational inefficiencies to providing quality care. The lack of mental health parity undeniably has a negative impact on counties, yet we remain firm in our position to work around these challenges and ensure the wellbeing of our communities.
Cost Per Bed Comparison: RTPs vs. RCCs
For more information explore our report:
Overcoming Barriers for Equitable Care Access: How the IMD Exclusion Impacts Counties.
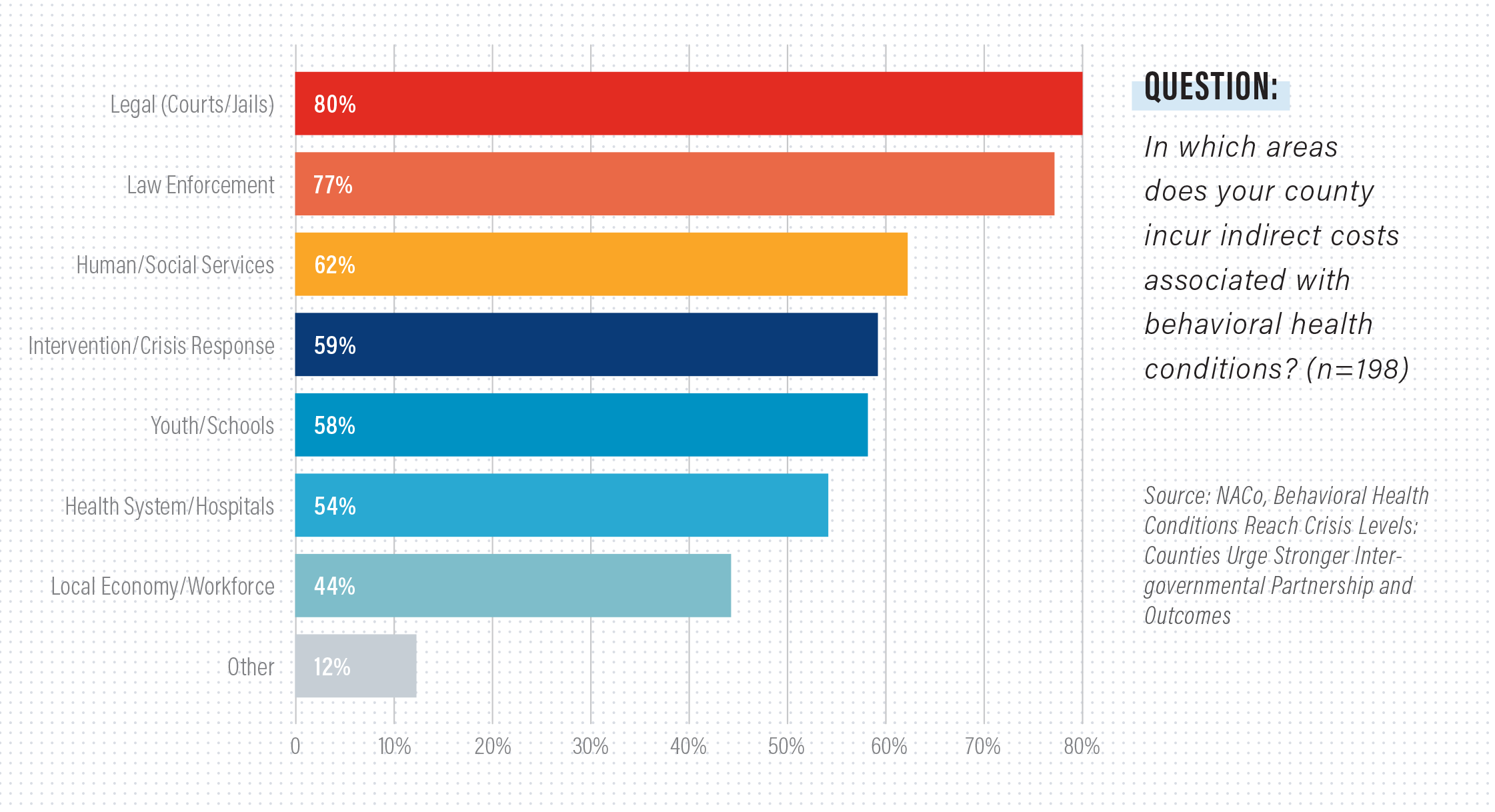
Our nation’s lack of an effective and widely available behavioral health services system has contributed to tragic outcomes for people in crisis. Not only does this have real-life negative impacts on our residents, it also drives up costs for the public sector and taxpayers that must bear the
financial burden when an individual is hospitalized or incarcerated. In a recent NACo survey, 80 percent of counties indicated that the county incurred indirect costs associated with behavioral health conditions through courts, jails and law enforcement.
Counties are implementing and testing new models of crisis care that are tailored to fit the unique needs of our communities. These models include tiered and co-response models, integrative care, wraparound services, referral systems and 24/7 call centers that support the recently implemented 988 Suicide & Crisis Lifeline. The long-term success of these efforts is dependent on strong intergovernmental and cross-sector partnerships, where all levels of government and community providers are invested in aligning systems for better outcomes for individuals in crisis.
A crisis response framework created by the Substance Abuse and Mental Health Services Administration (SAMHSA) recommends communities build infrastructure that provides someone to contact (988 Suicide & Crisis Lifeline), someone to respond (mobile crisis teams) and a safe place for help (specialized stabilization supports).
The Commission made significant progress in securing federal support to build and enhance the local crisis response infrastructure. Key achievements include:
- Enhanced accessibility to the 988 Suicide & Crisis Lifeline: Since its launch in 2022, the 988 lifeline has received over seven million calls, highlighting the pressing need for mental health support across the county. In March 2024, heeding the call of the Commission, the FCC proposed a new rule to georoute 988 calls based on the caller’s general location rather than the area code of the caller’s phone number, a similar approach to the one used in 911 call centers. By georouting calls according to the originating cell tower, the system directs calls to nearby crisis centers, enhancing response efficiency while maintaining caller privacy.
- Advanced intergovernmental consensus on crisis service policy: In May 2024, members of the Commission hosted a roundtable to modernize the National Guidelines for Behavioral Health Crisis Care by leveraging county best practices shared by SAMHSA, the Centers for Medicare & Medicaid Services (CMS), the Health Resources and Services Administration (HRSA) and other agencies. The roundtable featured exemplary county initiatives in financing, workforce development, accountability, integrated care and youth services, highlighting effective strategies for crisis care. Additionally, the roundtable explored how to incorporate county-driven approaches into the updated federal guidelines to improve crisis care services nationwide.
Travis County’s commitment to transforming behavioral health care into a readily available emergency resource is apparent the minute 911 dispatchers ask, “Are you calling for police, fire, EMS or mental health services?”
In 2019, Travis County expanded its partnership with Integral Care, the local mental health and intellectual and developmental disability authority, creating the Crisis Call Diversion Program (CCD), which introduced co-location in its 911 public safety answering point (PSAP) centers. In under six weeks, Travis County shifted some of the employees from Integral Care’s Expanded Mobile Crisis Outreach Team (EMCOT) to new roles as crisis center clinicians (C3s). Crisis center clinicians serve as trained behavioral health experts embedded within 911 PSAP centers.
Travis County introduced a call tree to assess eligibility to divert calls to C3s. This call tree prompts 911 dispatchers to ask whether weapons are present, if a crime is occurring and if other people are in immediate danger.
If the situation is deemed safe, the dispatcher passes the call to a C3, co-located in Travis County’s PSAP, to ensure a seamless transfer. Once on the line, a clinician draws from their specialized training to evaluate and provide appropriate care including de-escalation, emotional support and community resources. If an in-person response is needed, C3s can dispatch an EMCOT, offering in-person behavioral health support with or without law enforcement and EMS.
In only three and a half years, the program increased its full-time employees from 6.5 to 19; staff are now available 24 hours a day, 365 days a year. In 2023, C3s handled 6,292 calls (an average of 17 calls per day) and diverted 86 percent of calls away from law enforcement, reducing the demand on law enforcement while streamlining access to behavioral health care for Travis County residents. Looking forward, the county seeks to improve its technology and data-sharing abilities between C3s and law enforcement agencies to provide the best possible care in times of crisis.
Since 2020, Lewis and Clark County partners have been working on strengthening its Behavioral Health Crisis System Response, Stabilization and Diversion capacity, allowing more residents to connect to holistic and equitable support for behavioral health and substance use services. All three of the crucial components from the Crisis Now Model are at the core of these initiatives:
- A Person to Call: In July 2022, Lewis and Clark County and the state of Montana joined the rest of the United States in using the 988 Suicide & Crisis Lifeline. As of February 2024, Montana 988 received 1,077 behavioral health calls, de-escalating 885 (82 percent) of them, with only 140 (13 percent) requiring higher-level care.
- A Person to Respond: Lewis and Clark County, in partnership with St. Peter’s Health, launched a Mobile Crisis Response Team (MCRT) in 2020. Often, the team de-escalates crisis situations with law enforcement co-response, which previously may have resulted in the person in crisis being detained in jail. MCRT now evaluates the mental health needs of individuals in crisis for community treatment or emergency room admission. The MCRT consists of mental health professionals who respond directly to crises. In 2023, the team handled 347 incidents. The Mobile Crisis Response Team diverted 47 percent of crisis incidents from jails, with 71 percent resulting in community dispositions (home, public setting, group home) and 18 percent requiring emergency room visits.
- A Safe Place for Help: The Journey Home Crisis Stabilization Facility will be a critical community-based service for adults needing mental illness and substance crisis care. This upcoming eight-bed facility, set to open in 2024, will offer 24-hour receiving and three-to-seven-day stabilization services. It aims to further reduce detention center usage and emergency room visits by providing a safe place for crisis stabilization.
By focusing on these pillars, Lewis and Clark County is building a more responsive and supportive behavioral health crisis system, ensuring residents have better access to compassionate care and positive outcomes.
Calls to Montana 988

Lewis and Clark County hosts a real-time data dashboard to highlight information about its crisis response continuum.
Over 30 percent of the U.S. population resides in counties designated as having a mental health professional shortage. Counties are finding creative ways to increase and supplement the mental health workforce through positions such as certified peer support specialists, yet sometimes face policy barriers to full implementation. Counties are also seeking innovative strategies and opportunities to cover living expenses during training for those interested in joining the behavioral health workforce through apprenticeships, stipends and other paid training programs instead of just offering forgiveness of training and student loans after the fact.
Counties need direct and flexible resources to support the recruitment, training and retention of a sufficient behavioral health workforce. We need our federal partners to supplement local investments made in the behavioral health workforce through the enhancement of existing programs that promote workforce recruitment and retention. New financial incentives for integrated care will encourage more individuals to pursue jobs in the behavioral health care field and increase access to these critical services.
The NACo Commission on Mental Health and Wellbeing identified behavioral workforce issues as a signature policy issue. Key federal policy achievements include:
- Built partnerships with practitioners: Commission members partnered with behavioral health professionals and practitioners for a roundtable discussion in July 2023 on workforce priorities, with a significant focus on recruitment, retention and partnerships. Key themes included innovative strategies to fill vacancies, the importance of community and educational partnerships and the integration of peer support specialists. Discussions also highlighted the need for systemic changes such as policy reforms and improved funding mechanisms to sustain mental health services, particularly in rural areas. The roundtable underscored the critical role of collaboration between local governments, health care providers and educational institutions in enhancing mental health infrastructure.
- Advanced key legislation: In September 2023 the Bipartisan Primary Care Workforce Act, an important vehicle for Commission workforce priorities, passed out of the Senate Health Education, Labor and Pensions Committee. The legislation would strengthen primary care services by enhancing workforce development, expanding telehealth, investing in community health centers and addressing health disparities.
- Developed framework for intergovernmental alignment on policy solutions: Commission members highlighted workforce enhancement priorities with SAMHSA, HRSA and other federal agencies in a May 2024 roundtable discussion. These include continuing education, targeted recruitment strategies, workforce pipelines for specific populations, cost of living supports, cultural linguistics competency and early career pathways through high school internships.
Tulsa County, innovative approaches to behavioral health services are addressing the workforce shortage while providing essential support to individuals with severe mental illnesses. Programs of assertive community treatment (PACT) exemplify an evidence-based service delivery model that offers intensive, outreach-oriented mental health services. PACT teams operate 24/7, delivering comprehensive treatment, rehabilitation and support directly to clients in home and community settings.
The inclusion of peer providers, as defined by SAMHSA, enhances PACT’s effectiveness. Certified peer specialists, peer support specialists and recovery coaches use their lived experience of recovery from mental illness and/or addiction, coupled with formal training, to deliver services that promote mind-body recovery and resiliency. Their role is pivotal in guiding PACT staff during client intake, ensuring services are courteous, helpful and respectful.
Furthermore, Tulsa County benefits from the services of two community mental health centers (CMHCs): Family and Children’s Services and Counseling and Recovery Services, that receive funding from the Oklahoma Department of Mental Health and Substance Abuse Services. The centers provide peer services that are crucial for creating supportive environments for individuals with concurrent mental health and substance use disorders, including those engaged with the justice system. Peers play a vital role in fostering a welcoming atmosphere, guiding clients through available community services and resources and facilitating communication between clients and treatment staff.
The utilization of peers in Tulsa County’s behavioral health services not only helps address the workforce shortage but also significantly improves the quality of care. By leveraging the unique insights and empathetic understanding of peer providers, Tulsa County’s behavioral health system fosters independence, dignity and a stronger community support network for its clients
In FY 2022, Counseling and Recovery Services of Oklahoma:
- Served 8,818 adults and 4,941 children
- 96 percent of clients were low/no income and received care regardless of ability to pay
- 75 percent of all agency clients saw a reduction in substance use
- 75 percent of those discharged were not readmitted
- 98 percent of newly admitted children did not require a referral to inpatient psychiatric care, and
- 633 hours of recovery support services (including peer support, skills training and reinforcement).
Source: Counseling & Recovery Services of Oklahoma. Publications: Stay informed. www.crsok.org/publications/
Despite legislative and executive policy advancements over the last decade, there are still inexcusable and preventative disparities in the coverage of mental illness and substance use disorders under both public and private health insurance plans, when compared with coverage for medical and surgical benefits. Furthermore, while Medicaid and Managed Care Plans must follow federal parity laws, Medicaid fee for service plans do not, inhibiting many individuals with low income and disabilities and other vulnerable populations from accessing potentially life-saving coverage.
Counties urge the federal government to enforce policies that ensure equal coverage of treatment for mental illness and substance use. The Mental Health Parity and Addiction Equity Act (P.L. 110-343) is a federal parity law that was enacted in 2008 and requires comprehensive standards for equitable coverage of mental illness and substance use disorder treatment and coverage of physical treatment. Strengthening behavioral health parity protections and enforcing existing protections is a critical component of improving coordination and integration of primary care and behavioral health care, as well as better addressing the behavioral and mental health needs of our residents more broadly.
The NACo Commission on Mental Health and Wellbeing identified mental health parity as a federal policy priority. Key achievements include:
- Advanced regulatory reform: In July 2023, Commission leaders joined President Biden to announce a proposed rule from the U.S. Departments of Treasury, Labor, and Health and Human Services aimed at strengthening the Mental Health Parity and Addiction Equity Act (MHPAEA). The proposed rule is designed to enforce these parity provisions more effectively. NACo commented on the proposed rule requesting greater clarity and flexibility to enhance local government compliance with these new rules.
- Enforcing parity compliance across all insurers: Future advocacy efforts will emphasize enforcing parity across all insurers – federal, commercial and non-federal governmental plans – and providing clear guidance, assistance and incentives to ensure compliance among all types of insurers.
Learn more about mental health parity
Although federal laws like the MHPAEA have laid the groundwork, many states are still in the process of enacting and enforcing parity laws that require equal treatment of mental and physical health conditions in insurance plans. Meanwhile, counties across the U.S. are taking proactive steps to bridge the gap in mental health services. Fairfax County, through programs like the Merrifield Crisis Response Center (MCRC), exemplifies how local governments can support mental health parity and ensure residents have access to essential mental health services.
The Sharon Bulova Center for Community Health is a critical resource for individuals experiencing mental health crises. The center operates as a part of the county’s Community Services Board, providing a range of services to address urgent mental health needs. It offers comprehensive services designed to stabilize individuals in crisis and connect them with ongoing support. Key services include one-on-one peer support, daily virtual and in-person peer support groups, recreational and therapeutic activities and assistance with accessing benefits such as housing, food stamps (SNAP) or other resources. The center also gives away food, clothing, winter gear and hygiene kits.
One of the standout features of the Sharon Bulova Center for Community Health is that many of its services are provided free of charge. This is particularly important in addressing the gap in insurance coverage for mental health services. By offering no-cost crisis intervention and stabilization, Fairfax County ensures that all residents, regardless of their insurance status, have access to essential mental health care. This approach helps mitigate disparities in mental health treatment accessibility and aligns with the goals of mental health parity.
Services provided at the center have a significant impact on the community through a reduction in emergency room visits, improved access to care, enhanced community safety and decreased involvement with law enforcement. Since 2016, over 2,800 people with mental illness have been diverted from potential arrests and interactions with law enforcement.
Since 2016, over 2,800 people with mental illness in Fairfax County have been diverted from potential arrests and interactions with law enforcement.
Learn more about the Merrifield Crisis Response Center
Commission members acknowledge the significant role that youth and other vulnerable populations have in the ongoing mental health crisis, with these groups often facing unique and compounding challenges. Young people, particularly those from marginalized communities or who are aging out of foster care or involved in the juvenile justice system, are experiencing heightened levels of stress, anxiety and depression exacerbated by social, economic and educational disruptions.
Other vulnerable populations, including people experiencing homelessness, people with substance use disorders and people with disabilities, are disproportionately affected by the mental health crisis. These groups often lack access to adequate mental health care and support systems, leading to a cycle of poor mental health outcomes and increased interaction with emergency services, including hospitals and the criminal justice system. Addressing the mental health needs of youth and vulnerable populations is crucial for developing comprehensive, equitable mental health strategies and reducing the overall burden on community resources.
- Develop best practices and standards for fostering collaboration among various stake holders, including mental health professionals, service providers for those with intellectual and developmental disabilities, caregivers, schools, child welfare systems, homeless service providers and the broader community. Increased collaboration prioritizes the wellbeing of our youth and vulnerable populations through greater access to specialized mental health services.
- Leverage early intervention opportunities centered on youth-focused mental health and substance use disorder prevention strategies as an upstream strategy for addressing the mental health needs of the broader community.
Learn more about effective youth-focused prevention
Burlington County is committed to becoming a stigma-free community by dispelling misconceptions about substance use disorders and mental illnesses. In the county’s latest effort to expand mental health and substance use prevention services, it launched Hope One for Youth, a new mobile outreach unit focused on serving children and teens.
This initiative builds on the success of the Hope One Mobile Outreach Unit, operated by the Burlington County Sheriff’s Office in collaboration with the Department of Human Services , the Health Department and staff from Virtua Health, Maryville Addiction Treatment Center and Deborah Heart & Lung Center. In 2023, the Hope One Unit reached over 4,100 individuals, offering training on overdose antidote use, referrals to recovery services and other resources for those struggling with substance use disorders.
The Hope One for Youth unit visits local schools, youth group meetings, houses of worship and community events to deliver presentations, distribute age-appropriate materials and educate teenagers, children and parents about mental health, substance use prevention, emotional wellbeing and stigma reduction. The county also leveraged opioid settlement funds to secure more than 120 overdose emergency kits. These kits, which contain the overdose reversal drug naloxone, have been distributed to high schools and libraries across Burlington County.
The success of the Hope One Mobile Outreach Unit underscores the promise of a brighter future for youth and vulnerable populations with the implementation of Hope One for Youth. By establishing a mobile outreach unit specializing in youth services, Burlington County is enhancing early intervention, preventative measures, increasing access to critical services and working to destigmatize mental health issues.
The collaborative efforts of NACo’s Commission on Mental Health and Wellbeing are focused on enhancing equity in services, reducing barriers and promoting wellbeing for everyone. However, to achieve equity in all areas of health, we must address disparities in access to timely and appropriate behavioral health services for all populations.
Behavioral health equity ensures that all individuals, regardless of background, have equal opportunities to access high-quality and affordable health care services and support that are culturally and linguistically responsive. SAMHSA reports longstanding disparities in access to mental health treatment and the type of treatment received, particularly in minority communities. In 2022, among adults aged 18 or older who had a major depressive disorder in the past year, Hispanic (49.7 percent) or Black adults (51.2 percent) were less likely than white (66.6 percent) or multiracial adults (68.6 percent) to have received mental health treatment in the past year.16
- Diversify the local workforce to enhance cultural competence and reduce the stigma associated with seeking mental health support.
- Address social determinants of health that impact an individual’s ability to access care, such as employment stability, housing conditions, insurance status and proximity to services.
- Leverage data to identify inequities and guide decision-making, ensuring programs and policies provide fair, just and impartial treatment for all individuals and communities.
- Engage directly with communities and individuals impacted by mental health disparities to develop tailored solutions, incorporating their experiences and perspectives to create effective interventions.
As an active participant in the NACo-supported Familiar Faces Initiative, Stepping Up, and the Safety and Justice Challenge, Minnehaha County has made significant strides in promoting mental health equity and access to services, particularly for high-needs residents who frequently cycle through jails, homeless shelters, emergency departments and other crisis services. A particular focus has been addressing the needs of Native American residents, who are disproportionately represented in jail bookings. With support from the MacArthur Foundation, the county is reducing local incarceration, targeting racial and ethnic disparities, advancing racial equity, strengthening community engagement and contributing momentum toward criminal justice system reforms nationally.17
Key initiatives include the Alliance Reentry Program, which offers intensive case management and support for high-needs residents with complex behavioral health conditions. This program connects individuals to employment, housing and other services, significantly reducing recidivism.
The Safe Home project provides long-term housing and support for chronically homeless individuals with alcohol addiction, using a Housing First model. This initiative improves the lives of participants and saves taxpayers approximately $1 million annually by reducing the use of county resources such as law enforcement and emergency services.
The Link, a community triage center opened in 2021, provides 24/7 crisis care as an alternative to jail for individuals experiencing behavioral health emergencies. This center is staffed by a multidisciplinary team that ensures continuous support and treatment for residents
These initiatives demonstrate Minnehaha County’s commitment to a holistic, “whole person” approach that addresses all social determinant of health – including medical, behavioral and socioeconomic needs – ultimately reducing reliance on jails and emergency medical services while promoting equitable access to mental health care.
Racial and Ethnic Disparities in County Jail Bookings
The Safe Home project has not only improved the lives of participants but also saved taxpayers approximately $1 million annually by reducing the use of county resources such as law enforcement and emergency services.
Racial and Ethnic Disparities in County Jail Bookings
Black residents make up 6.1% of the county population, yet 15.8% of jail bookings and Native American residents make up 2.8% of the population, yet 35% of jail bookings.
County leaders continue to build upon the successes and milestones of the Commission on Mental Health and Wellbeing through investments in our political, financial and human capital aimed at promoting the wellbeing of our residents. As we lead the way in addressing the nation’s mental health needs, we will rigorously test and evaluate our policies and practices, constantly innovating to promote better outcomes by:
- Substance Abuse and Mental Health Services Administration. 2023. Results from the 2022 National Survey on Drug Use and Health: A companion infographic (SAMHSA Publication No. PEP23-07-01-007). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/report/2022-nsduh-infographic
- Substance Abuse and Mental Health Services Administration. 2023. Results from the 2022 National Survey on Drug Use and Health: A companion infographic (SAMHSA Publication No. PEP23-07-01-007). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/report/2022-nsduh-infographic
- Substance Abuse and Mental Health Services Administration. 2023. Results from the 2022 National Survey on Drug Use and Health. Highlights for 2022 NSDUH by Race and Ethnicity. https://www.samhsa.gov/data/sites/default/files/reports/rpt42731/2022-nsduh-race-eth-highlights.pdf
- U.S. Department of Health and Human Services. 2023. Mental illness. National Institute of Mental Health. https://www.nimh.nih.gov/health/statistics/mental-illness#part_2632
- Centers for Disease Control and Prevention. (n.d.). Wisqars leading causes of Death Visualization Tool. Centers for Disease Control and Prevention. https://wisqars.cdc.gov/lcd/?o=LCD&y1=2021&y2=2021&ct=12&cc=ALL&g=00&s=0&r=0&ry=0&e=0&ar=lcd1age&at=groups&ag=lcd1age&a1=0&a2=199
- Health Resources & Services Administration. 2024. Designated Health Professional Shortage Areas Statistics.
https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport. - American Journal of Psychiatry
- U.S. Department of Justice. 2017. Indicators of Mental Health Problems Reported by Prisoners and Jail Inmates, 2011-12.
https://bjs.ojp.gov/content/pub/pdf/imhprpji1112.pdf. - Congressional Research Services. 2023. Medicaid’s Institution for Mental Diseases (IMD) Exclusion (CRS Report No. IF10222).
https://crsreports.congress.gov/product/pdf/IF/IF10222. - County of Los Angeles Department of Mental Health. 2019. Addressing the Shortage of Mental Health Hospital Beds: Board of Supervisors Motion Response. https://file.lacounty.gov/SDSInter/bos/supdocs/142264.pdf
- The budget for the Residential Treatment Programs project was $50,896,000 (https://file.lacounty.gov/SDSInter/bos/supdocs/141555.pdf), the approximate cost per each of the 80 beds was $636,200.00. The total cost of the Recuperative Care Center’s 48-beds facility was $20,537,000
(https://www.treasurer.ca.gov/chffa/meeting/2020/20200730/staff/7-csi-la.pdf), bringing the cost per bed to approximately $427,854.17. - National Association of Counties. 2023. Shaping Crisis Response Spotlight Series. https://www.naco.org/resources/shaping-crisis-response-spotlight-series.
- Health Resources & Services Administration. 2024. Designated Health Professional Shortage Areas Statistics.
https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport. - Recovery Program Solutions of Virginia. Merrifield peer resource center (MPRC). https://www.rpsva.org/recovery-centers/merrifield/
- Burlington County, NJ. Burlington County providing mental health support services with new hope one for youth unit.
https://www.co.burlington.nj.us/CivicAlerts.aspx?AID=2224 - U.S. Department of Health and Human Services. 2022 National Survey on Drug Use and Health (NSDUH) Releases. 2024.
https://www.samhsa.gov/data/release/2022-national-survey-drug-use-and-health-nsduh-releases - MacArthur Foundation. 2024. Minnehaha County Grantee Profile. https://www.macfound.org/grantee/minnehaha-county-10114822/
- National Association of Counties. 2024. Improving outcomes through coordinated health and justice systems.
https://familiarfaces.naco.org/resources/case-study-minnehaha-county-s-d/